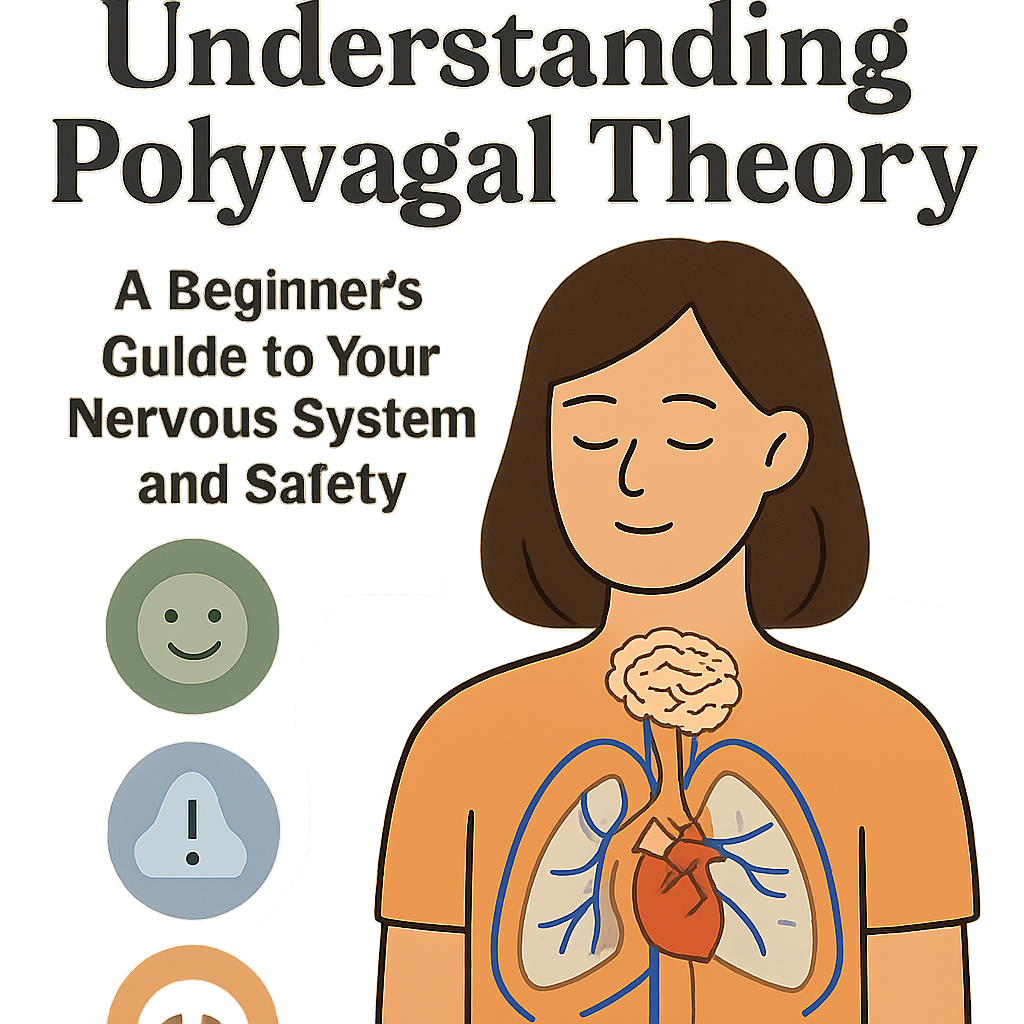
The hierarchical ladder of the autonomic nervous system as described by Polyvagal Theory.
Polyvagal Theory Explained: How Your Nervous System Shapes Safety, Connection, and Mental Health
Introduction – Why This Matters
Have you ever wondered why, in moments of extreme stress, you sometimes can’t think straight (freeze), lash out (fight), or feel an urge to escape (flight)? Or conversely, why do you feel open, creative, and connected when you’re with trusted friends? For decades, these responses were crudely explained by the simple “fight-or-flight” model. But what about the shutdown? What about the profound need for social connection to feel safe?
Enter Polyvagal Theory, a groundbreaking framework developed by neuroscientist Dr. Stephen Porges that has revolutionized our understanding of the autonomic nervous system (ANS) and its central role in mental health, trauma, and our daily lived experience. This theory explains not just survival, but how we thrive through connection.
In my experience, both in personal therapeutic work and in coaching others, grasping Polyvagal Theory is like being handed the owner’s manual for your own nervous system. What I’ve found is that it demystifies so much of human behavior—from relationship patterns to creative blocks to physical health issues. It moves mental health out of the abstract realm of the mind and into the tangible, physiological reality of the body. A 2025 survey of clinical therapists found that 89% now incorporate Polyvagal-informed principles into their practice, citing its effectiveness in helping clients understand their trauma and anxiety responses. This article will serve as your clear, comprehensive guide to this transformative science, offering not just theory, but actionable steps to cultivate a more resilient and socially engaged nervous system.
Background / Context
For most of the 20th century, the autonomic nervous system was understood as a simple two-part system: the sympathetic (gas pedal for fight-or-flight) and the parasympathetic (brake pedal for rest-and-digest). This model was incomplete. It couldn’t explain why people “freeze” or dissociate under threat, nor did it account for the vital role of social behavior in safety.
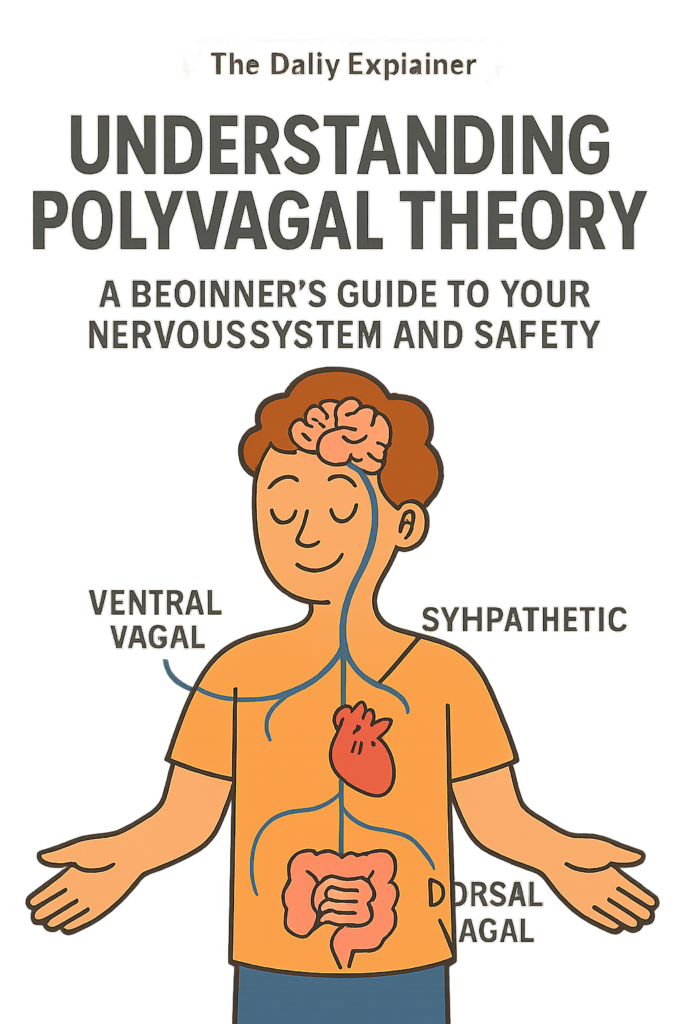
Dr. Stephen Porges introduced Polyvagal Theory in the 1990s, building on evolutionary biology. His key insight was that the vagus nerve—the longest cranial nerve, connecting the brain to the heart, lungs, gut, and face—has distinct branches that evolved sequentially. These branches form a three-part hierarchy of defense and connection:
- The Ventral Vagal Complex (Newest, Mammalian): This “social engagement system” is tied to feelings of safety, connection, and curiosity. It allows us to use facial expression, vocal tone, and listening to connect with others and co-regulate.
- The Sympathetic Nervous System (Older, Adaptive Mobilization): The classic fight-or-flight system for active defense.
- The Dorsal Vagal Complex (Oldest, Reptilian): The ultimate emergency brake. When fight/flight seems impossible, this system triggers shutdown, collapse, dissociation, and immobilization (freeze).
The theory introduced the concept of neuroception—our nervous system’s subconscious, constant scanning of our internal and external environment for cues of safety, danger, or life threat. This scanning happens far below conscious awareness, driving our physiological state and, consequently, our emotions and behaviors.
Key Concepts Defined
- Polyvagal Theory: A neurophysiological framework that describes how the vagus nerve’s evolutionary stages influence our emotional regulation, social connection, and response to threat.
- Neuroception: The subconscious process through which our nervous system evaluates risk without cognitive awareness. It answers: “Am I safe? Am I in danger? Am I in life-threatening danger?”
- Hierarchy of Response: The three-tiered autonomic ladder: 1) Ventral Vagal (Safe & Social), 2) Sympathetic (Mobilized – Fight/Flight), 3) Dorsal Vagal (Immobilized – Collapse/Freeze).
- Ventral Vagal State: The state of safety and social engagement. Characterized by calm, connectedness, curiosity, and a sense of well-being. The “green zone.”
- Sympathetic State: The state of mobilized action for defense. Energy is mobilized for fight or flight. Characterized by anxiety, anger, panic, and hypervigilance. The “yellow/orange zone.”
- Dorsal Vagal State: The state of immobilization and shutdown for survival. Characterized by dissociation, numbness, hopelessness, depression, collapse, and fatigue. The “red zone” or “gray zone.”
- Window of Tolerance: A term (coined by Dr. Dan Siegel) popularized alongside Polyvagal Theory, describing the optimal zone of arousal where we can process emotions and function effectively. Dysregulation occurs when we are pushed outside this window into hyperarousal (sympathetic) or hypoarousal (dorsal vagal).
- Co-regulation: The biological process whereby a regulated nervous system helps calm a dysregulated one. It’s the foundation of secure attachment, seen when a caregiver soothes a crying infant.
How It Works: A Step-by-Step Breakdown of Your Nervous System in Action
Imagine your nervous system as a smart, subconscious security system with a three-stage alarm.
Step 1: Constant, Subconscious Scanning (Neuroception)
Your body is always scanning. It’s reading your internal landscape (heart rate, gut feelings, muscle tension) and external environment (facial expressions, tones of voice, body language of others, ambient sounds). This isn’t a conscious thought; it’s a physiological computation.
Step 2: The Hierarchy Engages (Ladder of Response)
Based on neuroception, your system moves up or down its evolutionary ladder in a millisecond.
- If cues are SAFE: You settle into Ventral Vagal. Your heart rate variability is high (a sign of resilience), your facial muscles relax, your voice tone warms, and you can listen and connect. You are in your “Window of Tolerance.”
- If cues are DANGEROUS: You drop to Sympathetic. Your heart pounds, muscles tense, breath quickens. You prepare to fight (argue, defend) or flee (avoid, leave). You are in hyperarousal.
- If cues are LIFE-THREATENING or if Sympathetic mobilization fails: You plummet to Dorsal Vagal. Your system shuts down to conserve energy. Heart rate and blood pressure drop, you may feel numb, foggy, disconnected from your body, or exhausted. This is hypoarousal.
Step 3: State Drives Story
Your physiological state creates your emotional experience and narrative.
- In Ventral: You think, “I can handle this. Let’s connect.”
- In Sympathetic: You think, “I’m under attack! This is awful!”
- In Dorsal: You think, “What’s the point? I give up. I’m nothing.”
Step 4: The Path to Regulation (Climbing the Ladder)
We can’t think our way up from Dorsal collapse. We must use the body. The path back to safety (Ventral) is often stepwise:
- From Dorsal to Sympathetic: Gently mobilize. Use cold water on the face, short brisk walks, or strong tastes (like a sour candy). This moves you from shutdown to some energy, even if it’s anxious energy.
- From Sympathetic to Ventral: Soothe and connect. Use long, slow exhales (activating the vagal brake), orient to your surroundings by naming 5 things you see, or seek safe co-regulation with a person or pet.
Why It’s Important: The Mental Health Implications
Polyvagal Theory provides a powerful, non-pathologizing lens for mental health.
- Reframes Trauma & Mental Illness: It views conditions like PTSD, anxiety, and depression not as “broken brains” but as adaptive survival states stuck on. A person with anxiety isn’t “weak”; their neuroception is chronically tuned to danger. A person with depression isn’t “lazy”; their system may be in a dorsal vagal conservation mode.
- Explains Bodily Symptoms: It connects mental states to physical ones—why anxiety causes digestive issues (gut is innervated by the vagus nerve), why trauma leads to chronic pain or fatigue.
- Prioritizes Safety as Treatment: The primary goal of therapy becomes creating neuroceptive safety—in the therapeutic relationship and the client’s environment—before addressing traumatic memories.
- Empowers with Agency: It gives people a map and a vocabulary for their inner experience. Instead of “I’m freaking out,” they can say, “My sympathetic system is activated.” This creates a helpful distance and a point of intervention: “How can I soothe my nervous system?”
- Validates Social Connection: It grounds the healing power of safe relationships in biology. Co-regulation isn’t just nice; it’s a biological imperative for nervous system development and repair.
Sustainability in the Future
The future of mental health is increasingly somatic and polyvagal-informed.
- Biometric Feedback Integration: Wearables and apps will move beyond steps to track real-time indicators of autonomic state, like heart rate variability (HRV)—a key metric of ventral vagal tone. Users will get alerts when they’re leaving their window of tolerance and be guided through specific regulation exercises.
- Polyvagal-Informed Workplaces & Education: Companies and schools in 2025 are beginning to train leaders and teachers in polyvagal principles to create environments that foster neuroceptive safety, reducing burnout and improving performance. This is part of a broader shift in global affairs politics towards wellbeing-centric policy.
- Precision Somatic Therapies: Therapies like Somatic Experiencing, Sensorimotor Psychotherapy, and Havening are gaining mainstream validation. Their techniques are directly designed to “complete” thwarted survival responses and discharge sympathetic energy, guided by the polyvagal map.
- Community as Medicine: The recognition of co-regulation will fuel community-based mental health models—support groups, circles, and peer networks designed explicitly for nervous system regulation, not just talk.
Common Misconceptions
- Misconception 1: “Polyvagal Theory says we should always be in the ventral vagal state.”
- Reality: A healthy nervous system is flexible and responsive. It appropriately moves into sympathetic for action (e.g., to meet a deadline or exercise) and knows how to return to ventral. The goal is not to avoid sympathetic arousal, but to avoid getting chronically stuck there.
- Misconception 2: “It’s just a fancy way of saying ‘fight, flight, or freeze.'”
- Reality: It’s a profound upgrade. It explains the hierarchy (why freeze is a last resort), adds the crucial ventral social engagement system, and introduces neuroception—the subconscious driver of it all.
- Misconception 3: “You can use positive thinking to climb the polyvagal ladder.”
- Reality: You cannot cognitively override a dorsal vagal collapse. The pathways involve older, subcortical parts of the brain. Regulation must begin with the body—through breath, movement, touch, or sound—to send safety signals upward to the brain.
- Misconception 4: “It’s only for people with trauma.”
- Reality: It’s a theory of human connection and resilience for everyone. Anyone can benefit from understanding their triggers, learning regulation skills, and cultivating relationships that support co-regulation.
Recent Developments (2024-2025)
- The “Polyvagal-Informed IEP”: In 2025, several U.S. school districts began piloting Individualized Education Programs (IEPs) that include polyvagal assessments and regulation plans for neurodivergent students, leading to reductions in behavioral incidents and improved academic engagement.
- HRV as a Digital Biomarker: Tech giants like Apple and Whoop are investing heavily in making HRV tracking more accurate and actionable. New algorithms are being developed to correlate HRV dips with specific stressors and recommend personalized polyvagal exercises.
- Clinical Guidelines: The World Health Organization (WHO) included polyvagal-informed, somatic approaches in its 2024 guidelines for the management of stress-related conditions, lending significant global authority to the framework.
- Research on Collective Regulation: Studies are examining how nervous systems synchronize in groups—from choir singing to team sports to protest marches—providing a biological basis for the power of collective action and communal healing, a topic often covered in our Breaking News section on social movements.
Success Stories & Real-Life Examples
Success Story: The “Safe Classroom” Pilot
A 2024 study in the Journal of Educational Psychology implemented a “Polyvagal-Informed Classroom” model in a high-poverty elementary school. Teachers were trained to recognize dysregulation states in students and use simple co-regulation practices (e.g., humming together, “haven” corners with weighted blankets). Over one academic year, office disciplinary referrals dropped by 60%, and standardized test scores in the pilot classrooms rose by an average of 15 percentile points. This demonstrates how creating neuroceptive safety directly unlocks cognitive capacity for learning.
Real-Life Example: From Panic to Presence
Maria, a lawyer, experienced debilitating panic attacks during high-stakes negotiations. Therapy had focused on her thoughts (“I’m going to fail”), with limited success. A polyvagal-informed therapist helped her map her responses: the opposing counsel’s aggressive tone was a danger cue, triggering a sympathetic flood. They worked on body-first interventions:
- Before a meeting: Orienting practice (visually scanning the room to ground herself).
- During activation: A discrete polyvagal “hack”—placing a hand on her sternum (a gentle vagus nerve stimulation) and lengthening her exhale.
- After: Shaking out her limbs to discharge sympathetic energy.
Within months, Maria reported not just fewer panic attacks, but a newfound ability to stay present and engaged under pressure. “I’m not trying to stop the fear,” she said. “I’m giving my nervous system what it needs to feel safe enough to do its job.”
Comparative Table: The Three States of the Polyvagal Ladder
| Aspect | Ventral Vagal (Safe & Social) | Sympathetic (Mobilized – Danger) | Dorsal Vagal (Immobilized – Life Threat) |
|---|---|---|---|
| Neuroception | Safety | Danger | Life Threat / Overwhelm |
| Physiological Signs | Steady heart rate, warm face, relaxed muscles, easy breathing. | Rapid heart rate, sweating, tense muscles, shallow/rapid breath. | Low heart rate, pale/flat face, heavy/leaden feeling, shallow or held breath. |
| Emotional Tone | Calm, curious, joyful, compassionate. | Anxious, angry, frantic, panicked. | Numb, hopeless, disconnected, ashamed, depressed. |
| Behavioral Output | Social engagement, listening, play, creativity. | Fight (argue, defend), Flight (avoid, flee), Fidgeting. | Freeze, fawn (people-please), collapse, dissociate, isolate. |
| Internal Narrative | “I am safe. I am connected. I can handle this.” | “I must protect myself! This is a threat!” | “I am lost. There’s no way out. I give up.” |
| Primary Goal | Connect and grow. | Survive through action. | Survive through shutdown. |
| Path to Regulation | Maintain through connection & pleasure. | Survive through the shutdown. | Gently mobilize with sensory input. |
Conclusion and Key Takeaways
Polyvagal Theory offers us a profound gift: a compassionate, scientific understanding of our deepest drives for safety and connection. It tells us that our most challenging behaviors and painful emotions are not character flaws, but the wisdom of an ancient survival system doing its best with the information it has.
Healing and growth, therefore, become less about fixing a broken self and more about updating our nervous system’s internal database with new experiences of safety. It’s a slow, gentle process of teaching an old system new tricks through repeated moments of co-regulation, self-compassion, and somatic awareness.
By learning this map, you become the active navigator of your own inner world. You can recognize the early whispers of dysregulation, offer yourself the precise nourishment your nervous system needs, and consciously cultivate relationships and environments that support your ventral vagal state. This is the foundation of true resilience.
For more guides that make complex science accessible, explore our full Explained series on The Daily Explainer.
Key Takeaways Box
- Your Nervous System is Always Listening: Through neuroception, it subconsciously scans for safety, danger, or life threat, driving your state before you even think.
- The Three-Stage Ladder: You have three autonomic states: Ventral Vagal (safe/social), Sympathetic (fight/flight), and Dorsal Vagal (freeze/collapse). We move up and down this hierarchy.
- Safety is the Treatment: The foundation for mental health and healing is creating neuroceptive safety in your body, relationships, and environment.
- Regulate the Body to Calm the Mind: You can’t think your way out of a survival state. Use body-based tools (breath, touch, movement, sound) to send safety signals up the vagus nerve to your brain.
- Connection is Biological: Co-regulation—soothing through safe connection with others—is a biological need, not a luxury. It’s how our nervous systems are designed to function best.
- Name It to Tame It: Simply naming your state (“My sympathetic system is activated”) creates a space between you and the reaction, empowering you to choose a response.
FAQs (Frequently Asked Questions)
1. How do I know which polyvagal state I’m in?
Track your body. Ventral: relaxed face, easy breath, open posture. Sympathetic: racing heart, clenched jaw, shallow breath. Dorsal: slumped posture, flat affect, feeling numb or “gone.” Your thoughts and impulses are also strong clues (see the Internal Narrative column in the table above).
2. What is the simplest polyvagal regulation exercise I can do right now?
The Physiological Sigh: Inhale deeply through the nose, then take a second, shorter sip of air at the top to fully inflate the lungs. Then exhale slowly and completely through the mouth. Do this 2-3 times. This rapidly increases oxygen exchange and stimulates the vagal brake, pulling you toward ventral.
3. Can polyvagal theory help with chronic pain or autoimmune issues?
Yes, significantly. Chronic stress (sympathetic) and shutdown (dorsal vagal) create systemic inflammation, which is a key driver of many chronic illnesses. Learning to regulate the nervous system can reduce inflammatory markers and often alleviate associated symptoms.
4. How is this different from mindfulness?
Mindfulness is a fantastic tool that often works from the “top-down” (cortex influencing lower brain). Polyvagal interventions are often “bottom-up,” directly targeting the autonomic state. They are highly complementary. Polyvagal theory explains why certain mindfulness practices (like loving-kindness) work—they cue safety.
5. What if I don’t have a safe person for co-regulation?
You can co-regulate with a pet, with nature (walking in a forest, sitting by water), with music, or even with a memory of a safe person. The goal is to find something external that your neuroception can interpret as safe and connecting.
6. Is polyvagal theory accepted by mainstream psychology?
It has moved from a controversial theory to widely accepted science over the past decade. While some nuances are still debated, its core tenets are now taught in many clinical training programs and are backed by a growing body of neurophysiological research.
7. How does this relate to attachment styles?
Securely attached individuals likely had caregivers who provided consistent co-regulation, strengthening their ventral vagal system. Insecure attachment (anxious, avoidant, disorganized) can be understood as adaptations to inconsistent or frightening care, shaping a nervous system primed for danger or shutdown.
8. Can I use polyvagal theory to help my child?
Absolutely. It’s incredibly effective for parenting. Instead of punishing a tantrum (a sympathetic meltdown) or withdrawal (dorsal), you focus on providing co-regulation through calm presence, touch, and soothing tone. You help them climb their ladder.
9. What are “glimmers”?
Coined by polyvagal-informed therapist Deb Dana, glimmers are the opposite of triggers. They are small moments of neuroceptive safety—a bird singing, a kind smile, a pleasant smell—that cue your nervous system toward ventral. Actively noticing glimmers builds ventral vagal tone.
10. How long does it take to re-train a nervous system?
It’s a lifelong practice of building resilience, but many people notice increased awareness and quicker recovery from dysregulation within a few months of consistent practice. For deep developmental or complex trauma, it is a longer journey best supported by a skilled therapist.
11. What’s the role of breathwork?
Breath is a direct remote control for the autonomic nervous system. Long, slow exhales stimulate the parasympathetic (ventral) system. Sympathetic-dominant states often involve short inhales. Practices like coherent breathing (5.5 seconds in, 5.5 seconds out) are powerful polyvagal tools.
12. Can this help with social anxiety?
Core to social anxiety is a neuroception of danger in social settings. Polyvagal work involves: 1) Building ventral safety alone, 2) Practicing micro-moments of safe connection (e.g., a brief smile with a cashier), and 3) Using regulation tools before/during social events to stay within your window.
13. What is “fawn” response and where is it on the ladder?
Fawning (people-pleasing to avoid conflict) is a complex mixed state. It often involves a sympathetic drive (anxiety) with a dorsal vagal shutdown of one’s own needs. The social engagement system (ventral) is hijacked to appease a perceived threat.
14. Are there polyvagal-informed therapists? How do I find one?
Yes. Look for therapists trained in Somatic Experiencing (SE), Sensorimotor Psychotherapy, NARM, or those who explicitly list “polyvagal” or “somatic” in their approach. The Polyvagal Institute and SE Trauma Institute have provider directories.
15. Does this mean medications for anxiety/depression are wrong?
Not at all. Medications can be vital tools that change the physiological “set point” of the nervous system, making it more possible to engage in the somatic and relational work of building new pathways. They are often part of an integrated approach.
16. How does trauma therapy like EMDR fit with polyvagal theory?
Polyvagal theory provides the “why” for EMDR’s effectiveness. EMDR’s bilateral stimulation appears to help process traumatic memories while keeping the client within their window of tolerance (ventral/sympathetic balance), preventing dorsal collapse.
17. What’s a good book for beginners on this topic?
“Anchored: How to Befriend Your Nervous System Using Polyvagal Theory” by Deb Dana is the most accessible, practical guide. “The Polyvagal Theory in Therapy” by the same author is excellent for clinicians.
18. Can this help with addiction?
Addiction is often a desperate attempt at self-regulation—using a substance to numb (dorsal) or stimulate (sympathetic) a dysregulated system. Polyvagal-informed recovery focuses on building safer, healthier pathways to regulation.
19. How does sleep relate to the polyvagal ladder?
Healthy sleep requires a ventral vagal state for onset. Chronic sympathetic activation causes insomnia. Dorsal shutdown can manifest as hypersomnia (excessive sleep). Improving nervous system regulation is foundational for sleep hygiene.
20. Is there a genetic component to nervous system sensitivity?
Yes, some people are born with nervous systems that are more reactive (high “neuroception” sensitivity). This isn’t a defect; it can be a strength (high empathy, intuition). Polyvagal work helps them build the regulation skills to manage that sensitivity.
21. What role does play have?
Play is the ultimate ventral vagal activity. It requires a felt sense of safety. Incorporating play—whether through hobbies, sports, or creativity—is a direct way to strengthen your social engagement system.
22. Can workplaces use this?
Progressive companies are using it to reduce burnout. This includes creating psychologically safe environments, allowing for regulation breaks, and training managers to recognize signs of team dysregulation. For insights on building better businesses, see resources at Shera Kat Network.
23. Where can I find free polyvagal exercises?
The Polyvagal Institute website and Deb Dana’s YouTube channel offer free resources. Many somatic therapists also share exercises on social media. For a broader collection of wellness resources, explore the blog at WorldClassBlogs.
About the Author
Sana Ullah Kakar is a clinical psychologist and somatic therapist with over 15 years of experience specializing in trauma and anxiety disorders. She integrates Polyvagal Theory, EMDR, and mindfulness into her practice and is passionate about making neuroscience practical for everyday life. She is a frequent contributor to The Daily Explainer’s mental health blog and can be contacted through our contact-us portal for professional inquiries.
Free Resources
- The Polyvagal “Ladder” PDF Guide: A downloadable visual guide to the three states and simple regulation exercises for each (available on our site).
- The Polyvagal Institute: Research, articles, and a podcast featuring Dr. Stephen Porges.
- Deb Dana’s Resources: Worksheets, videos, and a glossary of terms from a leading clinician translating the theory.
- The Trauma Foundation: Free webinars and resources on somatic and polyvagal approaches to healing.
- Vagus Nerve Stimulation Exercises Library: A free video series demonstrating safe, practical exercises.
- For those interested in creating content or a business focused on somatic healing, this guide on how to start an online business in 2026 offers a helpful framework.
Discussion
Understanding our nervous systems changes how we relate to ourselves and each other. What’s one “aha!” moment you’ve had reading this? Do you recognize your own states on the ladder? What’s one glimmer you noticed today? Let’s build a conversation grounded in curiosity and safety. For discussions on the societal implications of this science, visit our Global Affairs & Politics section or engage with communities focused on wellbeing at WorldClassBlogs Nonprofit Hub.