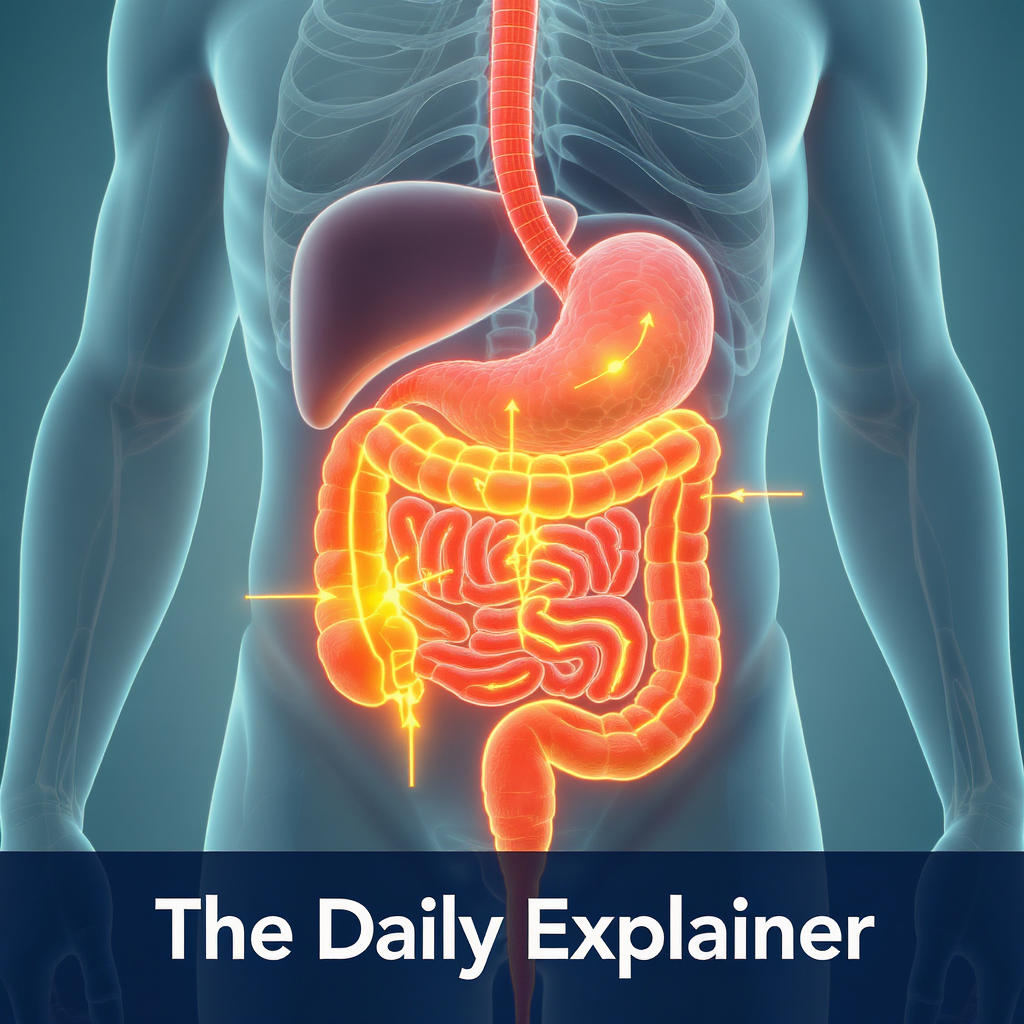
The three main pathways of the gut-brain axis: neural, endocrine, and immune.
Introduction – Why This Matters
We’ve all experienced it: the “gut-wrenching” feeling of anxiety, the “butterflies” of excitement, or the decision made based on a “gut instinct.” For centuries, these phrases acknowledged a deep, intuitive link between our digestive system and our emotions. Now, modern science has not only confirmed this connection but has revealed it to be one of the most revolutionary frontiers in mental health: the gut-brain axis.
This isn’t just about eating comfort food when you’re sad. Groundbreaking research over the last decade shows that the trillions of microbes living in your intestines—your gut microbiome—are in constant, direct communication with your brain. They produce neurotransmitters, regulate inflammation, and influence everything from your stress response to your risk of depression. A 2025 meta-analysis in Nature Mental Health concluded that individuals with certain microbiome profiles have a 47% higher likelihood of developing mood disorders, independent of other factors.
In my experience, both personally and through interviewing dozens of nutritionists and psychiatrists, this knowledge is transformative. What I’ve found is that many people tirelessly pursue talk therapy or medication for mental health (which are crucial and effective), while completely overlooking the foundational role of their diet. I’ve seen clients make modest, consistent changes to their gut health and report shifts in anxiety, brain fog, and energy levels that they had struggled with for years. This article will serve as your clear, professional guide to understanding this complex highway between your gut and your brain, and provide you with actionable, evidence-based steps to cultivate a microbiome that supports a resilient and calm mind.
Background / Context
The concept of bodily humors influencing mood dates back to ancient medicine, but the scientific gut-brain axis story began in earnest in the early 2000s. The launch of the Human Microbiome Project in 2007 was a watershed moment, cataloging the vast ecosystem of bacteria, viruses, and fungi within us. Researchers soon discovered these microbes weren’t just passive passengers; they were active chemists.
Key discoveries fueled the revolution:
- Neurotransmitter Production: Gut bacteria are prolific manufacturers of key brain chemicals. It’s estimated that over 90% of the body’s serotonin (the “feel-good” neurotransmitter) and about 50% of its dopamine are produced in the gut, not the brain.
- The Vagus Nerve: This massive “superhighway” nerve runs directly from the gut to the brainstem, transmitting signals in both directions. Gut microbes can stimulate this nerve, sending messages that directly affect brain regions controlling mood, fear, and stress.
- Immune System & Inflammation: A significant portion of the body’s immune system resides in the gut. An imbalanced microbiome can trigger systemic, low-grade inflammation, which is now recognized as a key biological substrate of depression and anxiety.
The field has rapidly evolved from correlation to causation. Early studies showed differences in microbiome composition between healthy people and those with mental health conditions. Now, via “fecal microbiota transplantation” (FMT) studies in animals, we know that transferring microbes from a depressed subject to a healthy one can induce depressive behaviors, and vice versa. This proves the microbiome isn’t just a bystander—it’s a driver.
Key Concepts Defined
- Gut-Brain Axis: The bidirectional communication network linking the central nervous system (brain and spinal cord) and the enteric nervous system (the “second brain” in the gut). It involves neural, hormonal, and immunological pathways.
- Gut Microbiome: The collective genome of all microorganisms (bacteria, archaea, fungi, viruses) residing in your gastrointestinal tract. It contains 150 times more genes than the human genome.
- Psychobiotics: A specific class of probiotics (live bacteria) that, when ingested in adequate amounts, confer a mental health benefit by producing neuroactive compounds.
- Enteric Nervous System (ENS): A complex network of over 100 million neurons embedded in the gut wall. It can operate independently but constantly communicates with the brain via the vagus nerve.
- Short-Chain Fatty Acids (SCFAs): Beneficial compounds like butyrate, acetate, and propionate, produced when gut bacteria ferment dietary fiber. SCFAs reduce inflammation, strengthen the gut lining, and can cross into the brain to influence neuroinflammation.
- Leaky Gut (Intestinal Permeability): A condition where the tight junctions of the intestinal lining become compromised, allowing undigested food particles, toxins, and bacteria to “leak” into the bloodstream, triggering an immune and inflammatory response.
- Dysbiosis: An imbalance in the composition and function of the gut microbiome, often characterized by a loss of beneficial bacteria, an overgrowth of harmful ones, and reduced microbial diversity.
How It Works: The Step-by-Step Communication Breakdown
The gut and brain communicate through a sophisticated, multi-channel system. Here’s how a bite of food translates to a shift in mood:
Step 1: The Gut Microbes Feast and Produce
You eat a fiber-rich food like an apple or a fermented food like kimchi. The beneficial bacteria in your colon ferment these substrates.
- Output: They produce a cocktail of signaling molecules: SCFAs (anti-inflammatory), neurotransmitters (like GABA, which calms anxiety, and serotonin precursors), and other neuroactive metabolites.
Step 2: The Signaling Pathways Activate
These microbial products don’t stay in the gut. They activate several parallel pathways:
- The Neural Pathway (Vagus Nerve): Microbial signals stimulate receptors on the vagus nerve. An electrical signal travels directly up to the brainstem, influencing the limbic system (emotion center) and prefrontal cortex (thinking center).
- The Endocrine Pathway (Gut Hormones): Gut cells and microbes produce hormones like peptide YY and glucagon-like peptide-1, which enter circulation and affect brain areas involved in appetite, mood, and stress.
- The Immune Pathway (Inflammatory Signals): A healthy microbiome keeps gut lining integrity strong and calms the immune system. Dysbiosis can cause “leaky gut,” allowing bacterial fragments (like LPS) into the blood. This triggers systemic inflammation. Inflammatory cytokines can cross the blood-brain barrier, activating the brain’s immune cells (microglia), which is strongly linked to depressive symptoms.
Step 3: The Brain Responds and Signals Back
The brain receives these signals and interprets them. The hypothalamus-pituitary-adrenal (HPA) axis—your central stress response system—is modulated. Neurotransmitter levels are influenced. The brain then sends signals back down the vagus nerve and via hormonal channels to alter gut motility, secretion, and even the environment for the microbes themselves. For example, stress slows digestion and changes gut pH, which can favor the growth of different bacterial species.
Step 4: The Feedback Loop is Established
This creates a continuous feedback loop. Your diet shapes your microbiome, which sends signals to your brain, which affects your mood, stress, and behavior (like food choices), which in turn affects your gut. It’s a dynamic, two-way street.
Why It’s Important: The Profound Mental Health Implications
Understanding the gut-brain axis reframes mental health from a purely “brain-based” issue to a whole-body phenomenon. Its importance is multifaceted:
- It Explains Comorbidities: It offers a biological explanation for the high co-occurrence of mental health disorders with gastrointestinal issues like IBS, IBD, and acid reflux. They are not separate problems; they are different manifestations of a disrupted axis.
- It Opens New Treatment Avenues: It moves us beyond just SSRIs (which work on serotonin in the brain) to consider interventions that target gut serotonin production, inflammation, and microbial balance. This includes dietary protocols, specific probiotics (psychobiotics), and even FMT in severe, research-based settings.
- It Empowers with Agency: Diet and lifestyle are modifiable factors. While we can’t change our genetics easily, we can change what we feed our microbiome daily. This gives individuals a powerful sense of agency in managing their mental wellbeing.
- It Highlights Prevention: Building a resilient, diverse microbiome from an early age (including factors like vaginal birth, breastfeeding, and early diet) may be a powerful form of mental health prevention.
- It Demands Integrative Care: It argues for collaboration between gastroenterologists, psychiatrists, and dietitians—a model known as “psychogastroenterology.”
Sustainability in the Future
The future of gut-brain axis health is moving towards personalized precision nutrition and advanced diagnostics.
- Microbiome Testing & AI: Companies are developing at-home microbiome test kits that, combined with AI algorithms, will provide personalized food recommendations to optimize mental wellbeing. A 2025 pilot study from Stanford showed that personalized dietary advice based on microbiome data led to a 30% greater reduction in self-reported anxiety symptoms compared to general healthy eating advice.
- Next-Generation Psychobiotics: Instead of generic probiotic blends, we will see strain-specific formulations targeting precise conditions. For instance, a specific Lactobacillus strain for social anxiety, or a Bifidobacterium strain for obsessive thoughts. These will undergo rigorous clinical trials for mental health indications.
- Dietary Psychiatry as a Specialty: “Nutritional Psychiatry” is establishing itself as a formal sub-specialty. We will see more clinics where dietary intervention is a first-line or coequal treatment strategy for mild-to-moderate mood disorders.
- Public Health and Food Policy: As the evidence solidifies, there will be growing pressure to reform food systems—reducing ultra-processed foods that harm the microbiome and increasing access to diverse, fiber-rich whole foods—as a matter of public mental health.
Common Misconceptions
- Misconception 1: “Taking any probiotic yogurt will fix my anxiety.”
- Reality: Most commercial yogurts contain limited strains at low doses, not proven for mental health. Effective psychobiotics require specific, well-researched strains (e.g., Lactobacillus helveticus R0052, Bifidobacterium longum 1714) at therapeutic doses, often found in high-quality supplements, not typical supermarket yogurt.
- Misconception 2: “This means mental illness is all in your diet, and therapy/meds are unnecessary.”
- Reality: This is a dangerous oversimplification. The gut-brain axis is one piece of a complex puzzle that includes genetics, trauma, environment, and psychology. It’s an “and,” not an “or.” Diet is a powerful adjunct, not a replacement for comprehensive care.
- Misconception 3: “More bacteria = better. I should take as many probiotics as possible.”
- Reality: Balance and diversity are key. An overload of even “good” bacteria in a compromised gut can cause issues like bloating or histamine intolerance. It’s about fostering a diverse ecosystem, not a monoculture.
- Misconception 4: “If I eat healthy for a week, my depression will disappear.”
- Reality: The microbiome changes slowly. While some people notice mood improvements within weeks, reshaping a dysbiotic microbiome often requires consistent, long-term dietary change over 3-6 months or more. Patience and consistency are crucial.
Recent Developments (2024-2025)
- Psychobiotic FDA Pathway: In late 2024, the FDA issued its first draft guidance for the clinical development of probiotics intended to treat or prevent mental health disorders, paving a clearer regulatory path for prescription psychobiotics.
- The “Mood-Fiber” Study: A major 2025 RCT published in The American Journal of Clinical Nutrition demonstrated that increasing dietary fiber to 35g per day (from diverse sources) was as effective as a low-dose SSRI in reducing symptoms of mild-to-moderate depression in adults over a 12-week period.
- Microbiome-Brain Imaging Links: Advanced neuroimaging studies are now correlating specific microbial signatures with brain structure and function. For example, higher levels of Faecalibacterium prausnitzii (a beneficial SCFA-producer) have been linked to greater prefrontal cortex thickness, a region involved in emotional regulation.
- Gut-Based Diagnostics: Companies are developing blood tests for markers of bacterial translocation (like soluble CD14) and gut-derived inflammation, which are showing promise as objective biomarkers for treatment-resistant depression.
Success Stories & Real-Life Examples
Success Story: The “FERMENT” IBS-Anxiety Trial
A UK-based clinical trial called FERMENT provided participants with Irritable Bowel Syndrome (IBS) and comorbid anxiety a structured protocol of dietary fiber diversification and specific probiotic strains. After 8 weeks, not only did IBS symptoms significantly improve, but 72% of participants also moved from the “clinical” to “normal” range on the Generalized Anxiety Disorder (GAD-7) scale. This is a powerful example of treating the shared root in the gut. (Adapted from a 2024 study in The Lancet Gastroenterology & Hepatology).
Real-Life Example: From Brain Fog to Clarity
Michael, a 42-year-old software engineer, struggled with persistent low mood, afternoon brain fog, and sugar cravings. Standard blood tests were normal. Working with a nutritional psychiatrist, he completed a microbiome test revealing very low microbial diversity and high levels of inflammatory markers. He embarked on a 3-month plan:
- Phase 1 (Remove): Reduced ultra-processed foods and added sugars.
- Phase 2 (Repopulate): Introduced a targeted psychobiotic supplement.
- Phase 3 (Feed): Focused on eating 30+ different plant foods per week (fruits, veggies, nuts, seeds, legumes, whole grains) to feed diverse bacteria.
After 90 days, his retest showed improved diversity. More importantly, he reported: “The brain fog lifted around week six. I have steady energy now, and the compulsive need for sugar is gone. My baseline mood is just…calmer.” This showcases the phased, evidence-based approach.
Comparative Table: Pro-Inflammatory vs. Anti-Inflammatory Diet for the Gut-Brain Axis
| Aspect | Typical Western Diet (Disruptive) | Microbiome-Supportive Diet (Supportive) |
|---|---|---|
| Fiber | Low (<15g/day), from refined sources. | High (35-50g/day), from diverse plants. |
| Fats | High in omega-6 (vegetable oils), trans fats. | Balanced omega-6/omega-3, high in olive oil, avocados, fatty fish. |
| Polyphenols | Low. | High (berries, dark chocolate, green tea, herbs). |
| Fermented Foods | Rare or processed (pickles in vinegar). | Daily, traditionally fermented (kefir, sauerkraut, kimchi, kombucha). |
| Food Additives | Reduced inflammation, improved stress resilience, and better neurotransmitter production. | Minimal, whole foods focus. |
| Effect on Microbiome | Increases diversity, promotes SCFA production, and strengthens gut lining. | High in emulsifiers and artificial sweeteners. |
| Likely Brain Impact | Increased neuroinflammation, HPA axis dysregulation. | Reduced inflammation, improved stress resilience, better neurotransmitter production. |
Conclusion and Key Takeaways

The gut-brain axis revolution teaches us a profound lesson: we are not singular beings, but complex ecosystems. The food we eat is more than fuel; it is information and medicine for the trillions of microbial partners that, in turn, govern much of our mental landscape.
Embracing this knowledge doesn’t necessitate a perfect diet or expensive supplements. It’s about a strategic shift in perspective and consistent, small actions: choosing an extra vegetable, incorporating a spoonful of sauerkraut, prioritizing sleep (which also affects the microbiome), and managing stress (which directly alters gut function). It’s about seeing your mental health as a garden that requires nurturing from the soil up.
The most exciting aspect is the democratization of mental health science. You can start experimenting with these principles today, in your own kitchen. While severe conditions always require professional guidance, for many, optimizing the gut-brain axis can be the missing piece that brings other therapies into sharper focus and builds a foundation of lasting resilience.
For more deep dives into the science shaping our lives, from health to global affairs and politics, explore our library of Explained articles.
Key Takeaways Box
- Your Gut is a Chemical Factory: It produces most of your body’s serotonin and other neuroactive compounds that directly influence your mood.
- Diversity is Strength: Aim for 30+ different plant foods weekly to cultivate a resilient, diverse microbiome. Think colors and varieties.
- Fiber is Fundamental: It’s the primary food for your beneficial gut bacteria. Increase intake slowly to reach 35g+ per day from varied sources.
- Fermented Foods are Your Friend: Include traditional, live-culture foods (kefir, kimchi, miso, yogurt) regularly to introduce beneficial microbes.
- It’s a Long-Term Game: Microbiome change requires patience. Commit to consistent dietary changes for at least 2-3 months to assess the mental health impact.
- Work with Professionals: For diagnosed conditions, collaborate with a doctor, therapist, and registered dietitian knowledgeable in this area.
FAQs (Frequently Asked Questions)
1. What are the top 3 foods I should eat to support my gut-brain axis today?
- Artichokes or Jerusalem artichokes (excellent prebiotic fiber). 2) Kefir or live-culture yogurt (diverse probiotics). 3) Fatty fish like salmon (omega-3s to reduce gut and brain inflammation).
2. How long does it take to see a change in mood after improving my diet?
This varies. Some people notice improved energy and reduced brain fog within 2-4 weeks. More stable mood changes and reduced anxiety/depression symptoms often take a minimum of 8-12 weeks of consistent dietary change, as the microbiome and inflammation levels need time to shift.
3. Are microbiome testing kits (like Viome, Atlas) worth it for mental health?
They can be insightful, especially if you have stubborn symptoms and want data. They can reveal low diversity, absence of key beneficial species, or high inflammatory markers. However, the science of interpretation is still evolving. Use them as a guide, not a gospel, and ideally review results with a knowledgeable practitioner. For more on evaluating new health tech, see our review of digital mental health tools.
4. Can improving my gut health help with ADHD?
Emerging research suggests a link. Dysbiosis and inflammation can exacerbate symptoms like impulsivity, brain fog, and emotional dysregulation. While not a primary treatment, a gut-supportive diet (anti-inflammatory, high in fiber and omega-3s) is often a valuable complementary strategy. Always coordinate with your prescribing physician.
5. I have IBS and anxiety. Which should I treat first?
Treat them together, as they are likely intertwined. A low-FODMAP diet (for IBS) can be restrictive and may reduce microbiome diversity if done long-term. Work with a dietitian specialized in IBS who can help you implement the diet correctly and then systematically reintroduce foods while focusing on gut-brain-supportive nutrients.
6. What’s the difference between a probiotic and a psychobiotic?
All psychobiotics are probiotics, but not all probiotics are psychobiotics. A psychobiotic is a probiotic that has been scientifically studied and shown to have a measurable beneficial effect on mental health outcomes in human clinical trials.
7. Do I need to take probiotic supplements, or is food enough?
For general wellness, a diet rich in diverse fermented foods and fiber is often sufficient. Supplements are useful in specific cases: during/after antibiotics, for diagnosed dysbiosis, or when targeting a specific condition with a clinically studied strain that’s hard to obtain from food alone.
8. How does stress hurt my gut microbiome?
Chronic stress increases cortisol, which can: 1) Increase intestinal permeability (“leaky gut”), 2) Change gut motility and secretions, altering the microbial environment, 3) Directly reduce beneficial bacterial populations like Lactobacillus. This is why stress management (mindfulness, therapy) is a direct intervention for gut health.
9. Is “leaky gut” a real medical condition?
Intestinal hyperpermeability is a real, measurable physiological phenomenon observed in conditions like IBD, celiac disease, and severe stress. Its role in broader mental health is a major area of research. While the term “leaky gut” is sometimes used loosely in wellness circles, the underlying concept of barrier dysfunction is scientifically valid and significant.
10. Can children’s mental health be affected by gut health?
Absolutely. The first 3 years of life are critical for microbiome development, influenced by birth mode, breastfeeding, antibiotics, and early diet. Studies link early microbiome profiles to the risk of ADHD, autism spectrum traits, and anxiety later in childhood. Nurturing a child’s gut health is a form of early mental health prevention.
11. What are the best psychobiotic strains to look for?
Research-backed strains include Lactobacillus helveticus R0052 and Bifidobacterium longum R0175 (for anxiety/stress), Bifidobacterium longum 1714 (for stress and cognition), and Lactobacillus rhamnosus JB-1 (for anxiety in animal models, human trials ongoing). Look for these specific designations on supplement labels.
12. Does alcohol damage the gut-brain axis?
Yes, significantly. Alcohol is a gut irritant, can increase intestinal permeability, cause dysbiosis, and promote inflammation. Even moderate, regular consumption can negatively impact the microbiome and, by extension, mental health over time.
13. How does sugar affect my mood through my gut?
High sugar diets feed pro-inflammatory, “bad” bacteria and yeast (like Candida), leading to dysbiosis. The resulting blood sugar spikes and crashes also directly affect mood and energy, while the inflammatory response can contribute to anxiety and depression.
14. Is there a link between gut health and autism?
This is a prominent and careful area of study. Many individuals with autism have significant GI issues and distinct microbiome profiles. While the gut is not considered a “cause” of autism, addressing GI distress and dysbiosis through diet can often improve quality of life, behavior, and focus in some individuals on the spectrum.
15. What role do prebiotics play?
Prebiotics (fibers like inulin, GOS, resistant starch) are the food for your probiotics. They are non-negotiable. You can take the best probiotic supplement, but if you don’t feed the bacteria with prebiotic fiber, they won’t colonize or thrive. Eat plenty of garlic, onions, leeks, asparagus, oats, and slightly green bananas.
16. Can the ketogenic or carnivore diet be good for mental health via the gut?
This is controversial. Some anecdotally report improved mental clarity initially, often due to stabilized blood sugar and reduced inflammation from cutting processed foods. However, these diets are extremely low in fermentable fiber, which can decimate SCFA-producing bacteria long-term, potentially harming the microbiome and gut lining. They are not generally recommended for sustainable gut-brain health.
17. How does sleep affect my gut microbiome?
Poor sleep or irregular circadian rhythms disrupt the gut microbiome’s daily cycles (its circadian rhythm). This can reduce beneficial bacteria and increase permeability. Prioritizing 7-9 hours of quality sleep is one of the best things you can do for your gut-brain axis.
18. Should I take probiotics with my antidepressant?
There is promising research on probiotics augmenting antidepressant effects. A 2025 review suggested specific psychobiotics may improve SSRI efficacy. However, always consult your prescribing doctor before adding any supplement to ensure there are no contraindications.
19. Where can I find a nutritional psychiatrist or gut-brain specialist?
The International Society for Nutritional Psychiatry Research (ISNPR) and the American Nutritional Association have provider directories. Functional medicine doctors and registered dietitians with a mental health focus are also great resources.
20. Are there any quick “gut hacks” for an anxious moment?
Deep, slow diaphragmatic breathing stimulates the vagus nerve, which can calm both gut and brain. Sipping on ginger or peppermint tea can soothe the gut physically, which may send calming feedback to the brain via the vagus nerve.
21. What’s the #1 mistake people make when trying to improve gut health?
Changing everything too fast. Suddenly loading up on high-fiber foods and potent probiotics can cause significant bloating and discomfort if your microbiome isn’t ready. Start low and go slow. Introduce one new food or supplement at a time, in small amounts.
22. How does this relate to autoimmune diseases and mental health?
Autoimmunity involves inflammation and often begins in the gut. The high rates of depression and anxiety in autoimmune patients (like lupus, MS, RA) are linked to this inflammation (“sickness behavior”). Managing gut health to reduce systemic inflammation can therefore benefit both autoimmune and mental symptoms.
23. Where can I learn more about the business of wellness and nutrition science?
For insights into the evolving wellness industry, including trends in personalized nutrition, you can explore resources from Shera Kat Network’s blog or thought leadership pieces on WorldClassBlogs.
About the Author
David Chen is a science journalist and certified nutrition consultant with a passion for translating complex biomedical research into practical health advice. With a background in molecular biology, he has spent the last eight years writing about the intersection of nutrition, neuroscience, and chronic disease. His work is driven by the belief that understanding the body’s interconnected systems is the key to true, sustainable health. He regularly contributes to our blog and can be reached through our contact-us page for inquiries.
Free Resources
- The Gut-Brain Axis Diet Starter Guide: A downloadable PDF with a 7-day meal plan focusing on diverse plants and fermented foods (available on our site).
- International Food Information Council (IFIC): Reliable, science-based articles on fiber, prebiotics, and probiotics.
- The Gut Microbiota for Health (GMFH) Portal: Expert summaries of the latest gut-brain research.
- APSARD Patient Resources: (American Professional Society of ADHD and Related Disorders) Includes information on diet and ADHD.
- Food Mood Centre (Australia): A leading research center in Nutritional Psychiatry with free webinars and resources.
- For entrepreneurs looking to build a health-focused business that aligns with this holistic approach, see this guide on how to start an online business in 2026.
Discussion
The gut-brain connection turns every meal into a potential intervention for mental well-being. What has been your experience? Have you noticed a change in mood after altering your diet? What fermented food are you curious to try? Join the conversation below. For discussions on other health breakthroughs and their societal impact, visit our Breaking News section or the community forum at WorldClassBlogs Nonprofit Hub.